A Comprehensive Guide To Pain and the Brain
Posted Nov 22, 2024 at 06:37
Posted Nov 22, 2024 at 06:37
Pain is an integral part of the human experience, serving as both a protective mechanism and a signal of underlying issues within the body. This blog explores the multifaceted nature of pain, delving into its definition, the relationship between pain and tissue damage, and the neurological implications associated with chronic pain.
The International Association for the Study of Pain (IASP) defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.” This definition emphasizes that pain is not merely a physical sensation; it encompasses emotional and psychological dimensions. Pain can be acute, resulting from a specific injury or illness, or chronic, persisting beyond the expected period of healing, often without a clear cause.
Pain is typically categorized into two main types:
One of the most intriguing aspects of pain is its relationship with tissue damage. While pain often signals actual physical injury, it can also be present in the absence of any identifiable damage. This phenomenon raises important questions about the nature of pain and how it is processed by the body.
In cases like chronic pain syndromes, individuals may experience significant pain even though medical examinations show no signs of tissue injury. For instance, people with fibromyalgia report widespread pain, fatigue, and cognitive difficulties, despite normal diagnostic tests. Similarly, neuropathic pain arises from damage or dysfunction within the nervous system itself, leading to sensations of pain, burning, or tingling without any associated tissue injury.
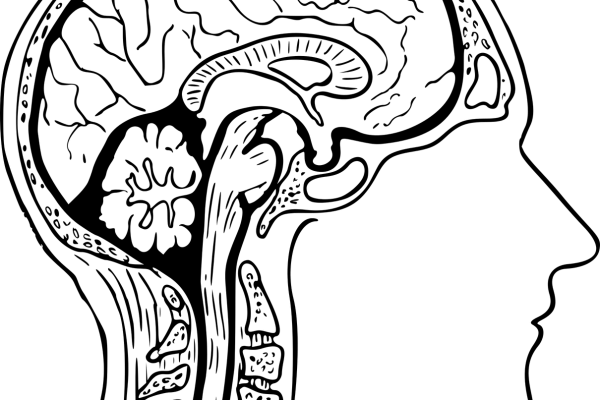
The perception of pain involves complex interactions between sensory nerves, the spinal cord, and the brain. When tissues are damaged, nociceptors (pain receptors) send signals to the spinal cord, which then transmits these signals to the brain for interpretation. However, the brain’s response can be influenced by various factors, including emotional state, previous experiences, and even social context.
Chronic pain has significant neurological implications, as it can lead to changes in the way the nervous system processes pain signals. These changes may contribute to the persistence of pain, even in the absence of ongoing injury.
One of the key mechanisms underlying chronic pain is central sensitization. This phenomenon occurs when the central nervous system (CNS) becomes hyperresponsive to sensory input, resulting in heightened pain sensitivity. In individuals with chronic pain, even normal stimuli that wouldn’t typically cause pain can be perceived as painful. This alteration in pain processing can lead to a vicious cycle, where pain begets more pain, further sensitizing the nervous system.
Research has shown that chronic pain can lead to structural and functional changes in the brain. For example, studies have indicated alterations in the size and activity of certain brain regions, including the thalamus and somatosensory cortex, which are involved in pain processing. These changes can affect emotional regulation, cognition, and overall quality of life.
Additionally, chronic pain is often associated with increased levels of stress, anxiety, and depression, further complicating the experience. This emotional distress can exacerbate pain perception and create a cycle that reinforces both psychological and physical suffering.
The brain uses various neurotransmitters to modulate pain perception. In chronic pain conditions, the balance of these neurotransmitters can become disrupted. For instance, increased levels of substance P (a neuropeptide involved in pain transmission) and decreased levels of serotonin and norepinephrine (which help regulate mood and pain perception) have been observed in individuals with chronic pain.
Pain is a complex experience that serves as a critical warning system in the body. Understanding its definition, the presence or absence of tissue damage, and the neurological implications of chronic pain is essential for effective management and treatment. As research continues to uncover the intricacies of pain perception and processing, healthcare providers can develop more targeted and effective interventions to improve the lives of those living with chronic pain. By acknowledging the multifaceted nature of pain, we can foster a more compassionate and informed approach to pain management, ultimately enhancing the quality of life for individuals affected by chronic pain conditions.